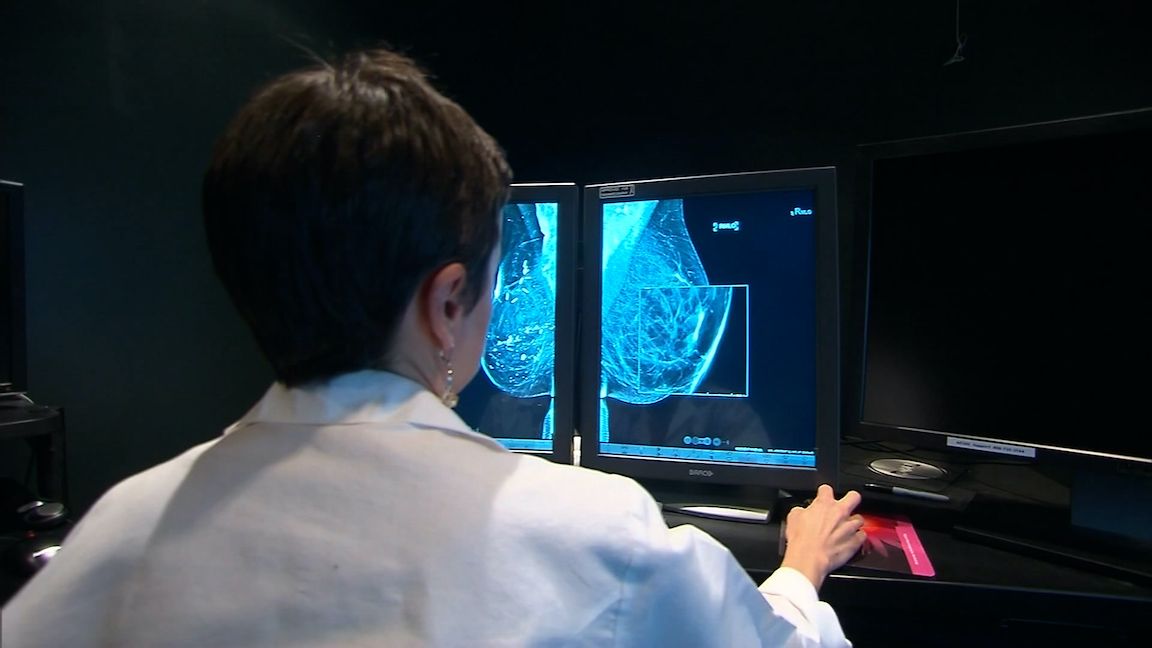
Newly proposed federal legislation aims to make supplemental breast cancer screenings more accessible.
U.S. Rep. Joe Morelle announced the new proposal at the Breast Cancer Coalition in Rochester.
It comes as the FDA introduced a new rule requiring all mammography reports and results letters sent to patients to include an assessment of breast density. Women with higher density, or a family history of breast cancer, require further screening. Many of them are forced to pay out-of-pocket for those tests, which can cost more than $1,000. Those who can't afford them often forgo those supplemental tests.
“The reimbursement from insurance has to be there for the hard-to-get screening tests that they need,” said Dr. Stamatia Destounis of Elizabeth Wende Breast Care. “And also if a patient gets called back for additional workup, whether it’s magnified views, whether an ultrasound or a biopsy, that’s all covered by insurance. Many of our patients are reluctant to come back for additional testing because they know they have to pay out of pocket for it.
The new proposal, called the Find It Early Act, would ensure all insurance plans cover those additional screenings.